Treating Eye Injuries Safely
We’ve had a lot of positive feedback on our last article about wearing proper protective eye equipment (PPE) when performing tasks that could be hazardous to your eyes. As we learned, there are only so many things in life that you can control, and wearing eye protection is one of them.
But what happens when you suffer an eye injury that is beyond your control?
The American Academy of Ophthalmology and Rand Eye Institute present some of the ways you can treat various eye injuries.

First step FOR ALL EYE INJURIES:
- Do not touch, rub or apply pressure to the affected eye.
- Do not try to remove the offending object from the eye.
- Do not apply ointment or medication to the eye.
- See an ophthalmologist or a medical doctor as soon as possible.
For a cut or puncture of the eye:
- Do not rinse with water.
- Do not remove the wedged/protruded object from the eye.
- Do not rub or apply pressure.
- Try loosely taping a paper cup or eye shield over the eye for protection; then seek help from a medical professional.
- Do not take aspirin, ibuprofen or other non-steroidal, anti-inflammatory drugs as these thin the blood and may increase bleeding.
For a liquid substance in the eye, or a chemical burn:
- Rinse your eye under a steady stream of warm, fresh water for 15 minutes. Just let it run into your eye and down your face.
- After rinsing, you can put a cool, moist compress or an ice pack on your eye, but don’t rub it.
- Call your eye doctor or emergency clinic to ask what is recommended for your injury. Tell the person what kind of substance got into your eye and what you’ve done about it so far.
A direct hit to the eye, from a ball or hard object:
Apply a small cold compress, gently, to reduce pain and swelling. Do not apply any pressure.
If a black eye, pain or visual disturbance occurs after a light blow, contact your eye professional or visit an emergency room right away.
Getting particles or foreign materials in the eye:
- Do not rub the eye.
- Carefully lift your upper eyelid. Blink several times to allow tears to flush the particles. If you have sterile eye drops, try using them. If the particles remain, keep the eye closed and seek medical attention right away.
As a precautionary measure, contact your ophthalmologist or eye doctor for additional assistance. Your doctor may need to see you right away, or suggest you visit an emergency clinic at once. It’s always safest to have someone drive you, even if you think you’re ok to drive. Always err on the side of caution because we only get ONE pair of eyes.
What is PPE? It’s Insurance for your Eyes
You’ve no doubt heard of a PPO and an HMO, but have you ever heard of a PPE?
PPE stands for “Personal Protective Equipment”, and it refers to clothing, footwear, goggles, gloves, helmets and other garments designed to protect us from injury or infection. But since March is Workplace Eye Wellness Month, let’s just concentrate on our eyes.

All joking aside, protecting your vision is paramount in maintaining quality of life, like seeing your grandkids or going for a leisurely Sunday drive.
Please don’t risk injury for vanity. Industrial Safety and Hygiene News reports that 70% of total eye injuries are a result of flying particles, flying or falling objects or sparks that strike the eye. Though companies can offer you eye protection and education, it’s up to you to actually put them to use.
Starting a new job? Helping a co-worker with a chemical or assisting in the construction of a project at work or home? It only takes one mishap for a life-changing event to happen that could cause you to lose your vision. Always make a note of where eye protection is located, familiarize yourself with the instructions, and most importantly, actually wear the eye protection. It’s 10-seconds of safety that could save your vision and your life.
Next time, we’ll talk about recognizing and treating eye injuries.
Relieving Eye Stress in the Digital Age
When people think of eye injuries at work, many conjure up the jobs that seem most risky to the eyes, like welder, construction worker, or chemical engineer (handling chlorine, acid and other chemicals). These are the types of jobs with the highest risk of having a foreign object enter the eye.
While those jobs do involve risk to the eyes, this month during Workplace Eye Wellness Month, we take a look at a more recent threat to our vision thanks to technology and convenience.
According to Pew Research Center, 77% of Americans own a smartphone, up from 35% in 2001. For many, this is the primary way they access digital information, via texting, email, engaging in social media platforms and surfing the web. Between smart phones, laptops and digital pads, nearly everyone in the U.S. is online some time during the day or night, and your eyes know it. Not so “smart” says The American Academy of Ophthalmology.
There are some simple ways to get relief from Digital Eye Strain, also known as Computer Vision Syndrome.
- Observe the 20-20-20 rule: Every 20 minutes, take a 20-second break and look at something 20-feet away and rest your eyes for 15 minutes after two hours of continuous computer use.
- Make sure that you’re looking down toward your computer screen, optimally about 4-5 inches below eye level as measured from the center of the screen and 20-28 inches from the eyes. Use an anti-glare screen when possible.
- Lighting is important. Position the computer screen away from the glare of light sources, particularly overhead lighting and windows. Use blinds or drapes on windows and switch to lower wattage bulbs in your desk lamps.
- If you’re using a word processing program, you might be able to raise the % size of your font (as shown below in the upper right of figure A), without affecting your document format.

This visual adjustment is an easy way to work with larger font without reformatting.
- This is a simple one: make an effort to blink frequently, keep eye drops by your side and stay hydrated by drinking plenty of water.
If you have uncorrected vision problems, it can increase the severity of Digital Eye Strain or Computer Vision Syndrome. Make an appointment with your eye care professional to see if there’s anything that can be done to improve your vision and comfort while using digital devices.
Next time, we’ll explore Personal Protective Equipment for your eyes, or PPE.
Tips for Self-Checking Your Vision for AMD
February may be the shortest month of the year, but it turns out to be the month we recognize the biggest cause of vision loss: Macular Degeneration, or AMD. More than 10-million Americans are affected by AMD, that’s more than people affected with cataracts and glaucoma combined.
The truth is that you or someone you love can be at risk for macular degeneration. Let’s outline some of the ways to see if you have the beginning stages of AMD, the leading cause of blindness in Americans 60 and older.
The first indication could be what you see or don’t see:
- Early signs of AMD include blurred vision and trouble distinguishing color and fine details.
- Difficulty seeing when going from bright light to low light and the need for increasingly brighter light to see up close.
- Colors appear less vivid and the vision is often hazy, or you see a blank or blurry spot in your central vision.
As the condition worsens, you could even lose your center of vision. Source AAO.
The Best Defense Against AMD is a Good Offense
The American Macular Degeneration Foundation recommends that you test your vision using The Amsler Grid (figure A below). It’s a lined graph that helps you determine if you have AMD.

(Figure A)
Figure A above is the normal Amsler Grid. Wear your reading glasses and look at the grid holding it 12 to 15 inches away from your face in good light following these instructions. You can print the grid here:
- Cover one eye.
- Look directly at the center dot with the uncovered eye and keep your eye focused on it.
- While looking directly at the center dot, note whether all lines of the grid are straight or if any areas are distorted, blurry or dark.
- Repeat this procedure with the other eye.
- If any area of the grid looks wavy, blurred or dark, contact your ophthalmologist.
- If you detect any changes when looking at the grid, you should notify your ophthalmologist immediately.
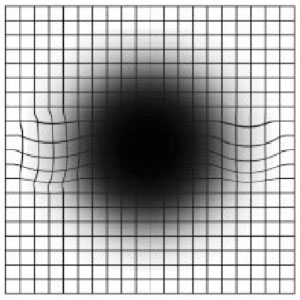
(Figure B)
Figure B above is the way the chart could look to you if you have age-related macular degeneration, with wavy lines and a black spot seen at center. Use the Amsler Grid to help you spot AMD early, so you can continue to enjoy clear vision.
Source: AAO
Macular Degeneration Wet vs Dry (AMD)
Imagine looking through a pair of dirty binoculars, a spyglass or a window that’s fogged up in the center. That’s what vision can look like to someone with macular degeneration.

Age-related macular degeneration or AMD, is the leading cause of blindness in people over the age of 60, it gradually diminishes central vision. Because detailed vision is processed by the macula, the central part of the retina, when the macula becomes damaged, daily activities like driving, reading and identifying faces become more difficult and eventually impossible.
There are two forms of macular degeneration: Wet and Dry
The dry form
The dry form is diagnosed in 85 to 90% of cases and it can occur in one eye or in both. The dry form is called “non-neovascular”, because it does not involve the leakage of blood or serum, but the deterioration of the retina, associated with the formation of small yellow deposits, known as drusen, under the macula.
The wet form
Though it occurs in only 10-15% of the cases, it results in 90% of the blindness associated with AMD. Wet AMD comes about when abnormal blood vessels begin growing behind the macula. These fragile vessels will leak fluid into layers of the retina (hence the name “wet” AMD), causing the macula to bulge or lift up from its normally flat position, distorting or destroying central vision. Vision loss from “wet” AMD may be rapid and severe.
While currently there is no cure for dry macular degeneration, those with wet macular degeneration may benefit from intraocular injections.
“With treatment, many patients have visual improvement and most patients are able to maintain their current vision without further vision loss. Without treatment, the condition usually worsens,” said Carl Danzig, MD, Director of Vitreo-Retinal Services at Rand Eye Institute.
AMD is one more reason why it’s so important to schedule a comprehensive dilated eye exam every 1-2 years.
Next time, we’ll suggest ways to test for AMD and offer some strategies for your best defense and prevention against macular degeneration, during Age-related Macular Degeneration Awareness Month.
Age-Related Macular Degeneration (AMD)
It’s February, The Month of Love, but let’s not wait until Cupid’s arrow falls to give our expressive eyes the respect and attention they so lovingly deserve.
February is the month that we pay special attention to Age-related Macular Degeneration (AMD), the leading cause of blindness among older Americans. The numbers are rising so high, so fast, that the American Macular Degeneration Foundation estimates that by 2030, 6.3 million Americans will be affected by AMD, the condition that limits a person’s ability to read and recognize faces.

As of today, there is no sure-fire cure for AMD, but there are some simple steps you can take to prevent it from happening to you:
Since AMD has no early warning signs, getting a regular comprehensive eye exam from an ophthalmologist is critical to diagnosing and treating AMD in its early stages. It is recommended that people over 65 have an exam every one to two years, even if they have no symptoms or eye problems.
Your family history plays a role in your future contact with AMD. If you have a close relative with AMD, you have a 50% chance of developing the condition. Speak with your family and research your family history for AMD. The earlier it is caught, the better the chance of saving your vision.
Diet plays a significant role in reducing AMD. Studies published in the American Journal of Epidemiology, Ophthalmology and Archives of Ophthalmology found higher levels of lutein and zeaxanthin in the diet are associated with a lower incidence of AMD. These include diets rich in omega-3 fatty acids such as fish. Maintaining proper weight and reducing your intake of saturated fats and cholesterol also helps prevent AMD. See these foods and recipes helpful in warding off AMD.
Quit smoking. This is always recommended whether you are at risk for AMD or not. Studies by the American Academy of Ophthalmology have shown that smokers are twice as likely to develop macular degeneration compared with non-smokers.
There are two types of AMD. In our next blog, we’ll define them both for you.
What can I do to prevent Glaucoma?
For Glaucoma Awareness Month, here are answers to the often-asked questions about early detection and prevention of this eye disease that affects more than 3-million people in the U.S., nearly half of whom are unaware that they have glaucoma. It’s time to become more aware.

What can I do to prevent Glaucoma?
Preventing glaucoma is only possible if you know that it’s oncoming. Since knowledge is power, early detection is critical. A comprehensive, dilated eye exam is the first crucial step to warding off this vision-stealing condition before it arrives and to halt its progression before irreversible damage occurs. Patients should have these exams beginning at age 40 and then every two years from age 65, with more frequent screenings if you’re in a high-risk category.
How Can I Determine my At Risk Factor?
Your family’s eye health history plays a huge role in determining whether you’re in a high-risk category. Being of African, Asian or Hispanic heritage can put you at higher risk, being over 40, having high eye pressure detected in an exam, being farsighted or nearsighted, or if you’ve experienced eye trauma or an eye injury. Those who have other health problems such as diabetes, migraines, high blood pressure or poor blood circulation should have regular eye exams to stay ahead of glaucoma.
Taking the Right “Steps”
Regular exercise may help prevent glaucoma, as it is known to help relieve pressure in the eye, so keep moving and help keep it away.
It’s Really a Cover-up
Wearing eye protection when working with power tools, splintering wood, welding or hammering can help prevent serious eye injuries that can lead to glaucoma. Wearing eye and head protection during sporting activity is also highly recommended, especially when participating in high-speed racquet sports.
Vision loss from glaucoma currently cannot be reversed; therefore the key is prevention and/or control. Please see your ophthalmologist or regular eye care doctor to schedule your comprehensive eye exam and leave glaucoma in the rear view mirror.
Glaucoma: Let’s Take the Pressure Off to Help You See Better
This month, the buzz is all about Glaucoma during National Glaucoma Awareness Month.
In last month’s blog, we explained glaucoma. Today we want to present some of the effective treatments for glaucoma, which is now one of the leading causes of blindness.
Because glaucoma is caused by increased pressure in the eye, the first plan of treatment is to lower the pressure within normal values.

Here are three main ways to accomplish this:
Eye Drops: The most common and convenient treatment for lowering intraocular pressure (IOP) inside the eye. Prescription eye drops can lower your IOP, offering a chance for the excess fluid to escape the eye via the trabecular meshwork/Schlemm’s canal (TM/SC) and the uveoscleral pathway. Ask your doctor to explain the options best suited for your condition.
Laser Surgery: This option is often suggested before the doctor will recommend incisional surgery. With laser surgery, a focused beam of light is used to help control the eye pressure, by enhancing the eye drainage function. In some cases, the laser treatment, known as iridotomy, is used to make tiny holes in the iris to help improve drainage, effectively lowering pressure in the eye.
Operative Surgery: When eye drops and laser surgery are not as effective, the doctor may suggest operative surgery to create a new bypass drainage tunnel. The fluid can properly drain through this new path allowing for pressure in the eye to reduce, offering relief and improved vision.
Rand Eye-Q tip: Reducing your intake of alcohol and caffeine are highly recommended options that can help stave-off glaucoma, and of course, smoking cessation is always great advice.
Consult with your ophthalmologist for the options best suited for you. Click here to schedule a comprehensive eye exam at Rand Eye Institute.
January is Glaucoma Awareness Month
See The New Year Crystal Clear!
Happy New Year! We hope you SEE happy times ahead in 2017 and we have some vision advice to help make that happen.
January is Glaucoma Awareness Month. Glaucoma is called “The Sneak Thief of Sight” because it occurs so gradually that you may not even be aware that you’re developing vision loss due to glaucoma.

Glaucoma occurs when pressure in the eye becomes higher than normal resulting in increased pressure on the optic nerve, pinching the blood vessels that carry blood to the retina and optic nerve.
While many people schedule a baseline screening every year or so, the BEST way to prevent glaucoma is with a comprehensive dilated eye exam. In a comprehensive eye exam, your eye pressure will be tested as well as the front part of your eye, retina and optic nerve.
Glaucoma is one of the leading causes of blindness but it doesn’t have to happen to you. Early testing and prevention are extremely important, especially since there is no known cure. There are three procedures that can help to stop or regulate glaucoma in its tracks. If diagnosed, your doctor can explain these options thoroughly and choose which is best suited for your condition:
- Prescription eye drops
- Laser surgery
- Filtration surgery
You don’t have to be elderly to be at risk from glaucoma, everyone from babies to senior citizens can be at risk, in fact, 1 out of every 10,000 babies born in the U.S. are born with glaucoma.
Here’s the key: When glaucoma is diagnosed early and treated adequately, it rarely ends in blindness. That’s why it’s so important to have regular eye exams. Click here to schedule an appointment at Rand Eye Institute.
New Year Fireworks – Eye Safety Tips
Whether you’re saying “Au Revoir” to 2016 or getting ready to welcome in 2017, we want to make sure you remember “safety first” when planning to be around fireworks this New Year’s Eve.
Practice fireworks eye-safety during your celebration: Keeping it safe and fun for the entire family.
- First and foremost, do not use illegal explosives, professional fireworks, or any fireworks that you did not obtain from a licensed retailer in your city. Unlicensed fireworks can be dangerous to you and your eyes, which may lead to eye trauma and blindness.
- Make sure the area where you will be lighting fireworks has a safe perimeter between you and the spectators, that it’s free of overhead obstructions and away from dry grass or flammable materials, including automobiles. Look out for flaming embers flying through the air that could land in your eyes.
- When igniting approved fireworks, always wear safety gloves and protective eyewear and never allow children to assist in engaging fireworks. You can easily obtain small, non-igniting battery-operated lit toys that the kids will enjoy.
- If you’re attending a professional fireworks display, like the ones hosted by your local city or town, remember, THEY’RE THE EXPERTS. Don’t bring your own fireworks, which in fact is usually against park rules.
The National Council on Fireworks has more tips here to help you safely ring in the New Year.